News
Isolating best brain stem cells to treat MS
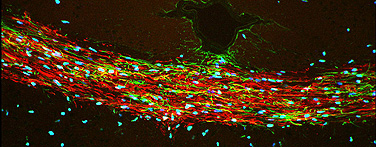
Areas in red indicate mouse brain cells coated with myelin, a crucial substance lacking in patients with MS.
-
 Print
Print -
 Comments
(1)
Comments
(1)
-
You need to have the right cells in hand before you can even think about getting to a clinical trial to treat people. This is a significant step.”
The prospect of conducting human clinical trials with stem cells to treat diseases like multiple sclerosis may be growing closer, say scientists at UB and the University of Rochester, who have developed a more precise way to isolate stem cells that will make myelin.
Myelin is the crucial fatty material that coats neurons and allows them to signal effectively. The inability to make myelin properly is the cause of MS, as well as rare, fatal, childhood diseases, such as Krabbe disease.
The research, published online and in the October issue of Nature Biotechnology, overcomes an important barrier to the use of stem cells from the brain in treating demyelinating diseases.
Until now, it has been difficult to separate out the right progenitor cells—the ones that will develop into cells that make myelin, explains Fraser Sim, first and co-corresponding author on the paper and assistant professor in the Department of Pharmacology and Toxicology, UB School of Medicine and Biomedical Sciences; Sim did much of the work while he was a researcher at Rochester.
“Characterizing and isolating the exact cells to use in stem cell therapy is one key to ultimately having success,” Sim says. “You need to have the right cells in hand before you can even think about getting to a clinical trial to treat people. This is a significant step.”
Sim and Rochester graduate student Crystal McClain ran extensive analyses looking at gene activity in different types of stem cells, leading to the conclusion that stem cells carrying a protein known as CD140a on their surface seemed to be most likely to become oligodendrocytes—the type of brain cell that makes myelin.
The UB and Rochester scientists then injected the cells into the brains of mice that were born without the ability to make myelin. Twelve weeks later, the cells had become oligodendrocytes and had coated more than 40 percent of the brain’s neurons with myelin—a four-fold improvement over the team’s previous results published in Cell Stem Cell and Nature Medicine.
“These cells are our best candidates right now for someday helping patients with MS, or children with fatal hereditary myelin disorders,” says Steven Goldman, co-author, team leader and professor and chair of the Department of Neurology at the University of Rochester Medical Center. “These cells migrate more effectively throughout the brain, and they myelinate other cells more quickly and more efficiently than any other cells assessed thus far. Now we finally have a cell type that we think is safe and effective enough to propose for clinical trials.”
An eventual treatment of a disease like MS might involve injecting stem cells to create myelin in the brains of patients.
“Another approach,” says Sim, “might involve using certain medications to turn on these cells already present in the brains of patients and thereby create new myelin. The use of the new techniques described in this work will permit us to better understand how human cells behave in the brain and help us predict which medications may be successful in the treatment of myelin loss.”
The new approach also may be applicable to Krabbe disease, Sim says, which also involves the breakdown of myelin. Sim, who came to UB in 2009, is actively collaborating on related work with researchers at the Hunter James Kelly Research Institute, a partnership between UB and the Hunter’s Hope Foundation and located in UB’s New York State Center of Excellence in Bioinformatics and Life Sciences.
In addition to Sim, McClain and Goldman, other authors of the paper are Martha Windream, assistant professor in the Department of Neurology, and technical associates Steve Schanz and Tricia Protack, all of the University of Rochester.
The work was supported by the National Institute of Neurological Disorders and Stroke, the National Multiple Sclerosis Society, the New York State Stem Cell Research Board, the Adelson Medical Research Foundation and the Mathers Charitable Foundation.

Reader Comments
James M. Mazur says:
My uncle has multiple sclerosis. I am excited to see where this research will lead!
Posted by James M. Mazur, Student, 10/25/11